


Joseph R. Anticaglia MD
Medical Advisory Board
Karen is a 52 year old IT worker who has been treated for several years because of hypertension, elevated cholesterol, and problems with her gallbladder (cholecystitis). When she complained of indigestion, and had pain in the upper part of the stomach that radiated to the back and neck, she thought it was another gallbladder attack. However, when she had chest tightness and trouble breathing, her husband took Karen to the hospital’s emergency department…
In the ED a medical history was obtained., physical examination performed, and blood was drawn, and sent to the laboratory for evaluation. An electrocardiogram was done as well.
The electrocardiogram indicated that she was having a heart attack (myocardial infarction). What was of particular concern was that the EKG finding in Karen’s case suggested a blockage of a medium or large coronary artery that supplies blood to the heart (STEMI-see glossary).
When the blood work came back from the lab there was, for example, an elevated troponin level, which is a cardiac enzyme (biomarker) that is released into the bloodstream soon after a person has a heart attack indicating damage to the heart muscle and a heart attack. Other blood enzymes were elevated which pointed to a heart attack.
The doctor advised doing a coronary angiogram, which is done to determine if a person has blockage or narrowing of the coronary arteries that supply oxygen and nutrients to the heart muscle. It is a method of obtaining X-rays of the heart’s blood vessels by injecting a special dye, contrast agent, into the heart’s blood arteries through a thin, flexible tube called a catheter.
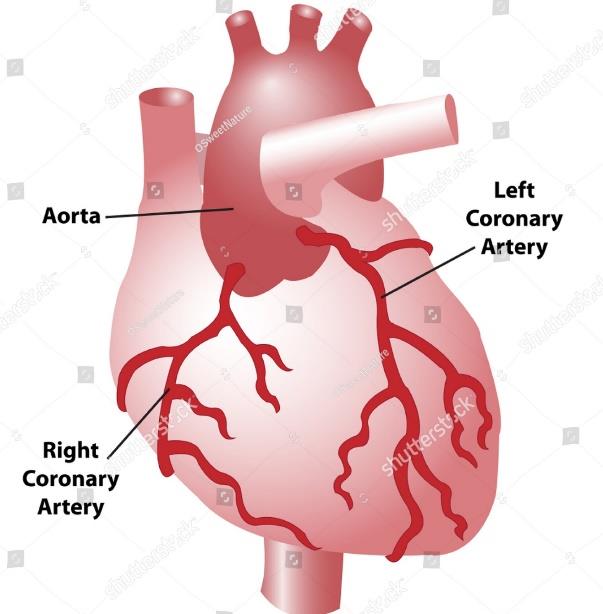
The dye highlights the blood vessels, allowing doctors to visualize the coronary arteries. Karen had blockage of two major coronary arteries; the right coronary artery was blocked 100 percent, and the left coronary artery was blocked 50 percent.
The left anterior descending (LAD) artery is the largest coronary artery. It sends nearly half of the oxygen-rich blood to the left side of your heart (to the left ventricle). This artery is also known as the widowmaker artery because blockage in it can lead to a fatal heart attack.
A coronary stent is a small, expandable, springlike metal mesh tube that’s used to treat narrowed or blocked coronary arteries. It restores blood circulation to the heart preventing or minimizing future damage to the heart muscle. It clears the blocked artery.
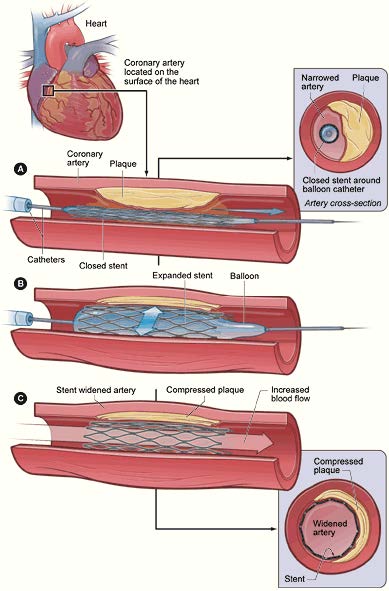
pWhen the stent is inserted into the coronary artery, it’s intended to be permanent and to last a person’s entire life. After placement of the stent, it may take three to 12 months for tissue to fully coat the stent. However, it’s possible the stented area can re-narrow. In those instances, another coronary stent is placed in the same location.
The body rejects foreign bodies such as BMS that can cause an inflammatory reaction which leads to re-narrowing, re-stenosis of the coronary artery. It can also predispose a person to form blood clots in the area of the stent.
Drug-eluting stents release medication into the artery’s wall over a few months to prevent re-narrowing of the coronary artery. The drug is coated around the stent. However, if the arteries narrow again, the procedure needs to be repeated. The second stent procedure usually happens within the first six months of the initial intervention.
Individuals need to control risk factors such as cholesterol levels, diabetes, hypertension , obesity, getting enough exercise, quit smoking and avoiding excessive alcohol intake.
Your physician will prescribe anticoagulants, blood thinners to minimize blood clot formation in the coronary arteries, as well as medications to control risk factors.
The placement of coronary stents have save countless lives. However, it is one part of the treatment plan. It’s incumbent on the individual to consult with his/her physician, to control risk factors so as to enjoy a better quality of life.
STEMI (ST elevation myocardial infarction) — with this finding on ECG, heart attacks are usually associated with a significant blockage of a main coronary artery.
Interventional cardiologist is a cardiologist who has received one or two years additional training in cardiology with the ability to perform minimally invasive catheter based procedures.
Angioplasty is a non-surgical procedure used to open blocked arteries in many parts of the body. It’s most commonly used to treat coronary artery disease to restore blood flow to the heart.
FFRCT, or Fractional Flow Reserved derived from CT is a non-invasive procedure that uses a CT scan of the heart to provide detailed information about blood flow through the coronary arteries that can help doctors diagnose and treat coronary artery disease (CAD).
Emre K. Aslanger, et al. Diagnostic accuracy of electrocardiogram for acute coronary occlusion resulting in myocardial infarction; Int J Cardiol Heart Vasc Oct 2020
American Heart Association; What is a Stent?
StatPearls; Coronary Artery Stents;
Heart Attack; Mayo Clinic, October 9, 2023
NSTEMI: Non-ST-Elevation Myocardial Infarction (Heart Attack); Cleveland Clinic, December 28, 2021
This article is intended solely as a learning experience. Please consult your physician for diagnostic and treatment options.